In the ongoing discussion about healthcare in the United States, one of the most significant recent topics has been the potential inclusion of the obesity-treating drug, Wegovy, under Medicare coverage. This development brings to the forefront questions regarding not just the efficacy of such treatments but also their broader economic implications on a system already burdened by escalating costs. Assessing the potential of Wegovy to be a cost-effective solution involves a nuanced understanding of its pricing, long-term health benefits, and the economic mechanics of Medicare.
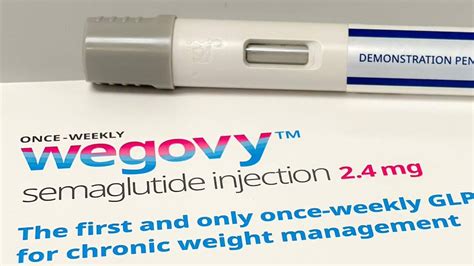
Wegovy, a high-cost medication priced at around $10,000 per year, is indicative of a larger dilemma in the healthcare system. The significant financial investment in such medications raises the question of value over time. Proponents argue that, despite the initial costs, medications like Wegovy could potentially save more money long-term by reducing the need for treatment of obesity-related conditions such as cardiovascular diseases, which are often more expensive and require intensive, ongoing healthcare services.
One of the critical elements in this discussion is the comparison of Wegovy with other preventative measures covered by Medicare, such as the HIV preventative medication, PReP. Both drugs come with high annual costs but promise significant long-term health care savings by preventing more severe diseases. The economic rationale is clear: investing early in preventive care can lead to overall savings. However, this raises questions about the pricing strategies employed by pharmaceutical companies and the role of Medicare in negotiating these prices to make such treatments accessible at a lower cost.
The potential side effects of Wegovy, while comparable to those of other medications in its class, also warrant attention. The history of pharmaceutical treatments for obesity includes instances like Fen-phen, which was discontinued due to its adverse cardiac effects. With any new medication, especially one that could be deployed widely via Medicare, understanding and monitoring for long-term side effects is critical to ensure it does not end up costing more in unforeseen adverse health outcomes.
Furthermore, international pricing comparisons shed light on the discrepancies in drug costs, possibly influenced by different regulatory and negotiating frameworks. For instance, the negotiated rate for Wegovy under Blue Cross in the U.S. is significantly higher than prices available in the UK and EU. These differences underscore the potential for Medicare to leverage its bargaining power more effectively, a recent development with the government gaining negotiation rights. Whether these negotiations will lead to substantial price reductions for Wegovy remains a question of strategic importance.
Beyond the numbers, there’s the societal and ethical dimension to consider. Obesity is a complex condition with multifactorial causes including genetics, lifestyle, and societal factors such as food availability and marketing. The focus on a pharmaceutical solution like Wegovy might overshadow necessary discussions and actions on these broader determinants of health. While the drug may provide a clinical solution to an individual’s health, it does not address the root causes of obesity on a societal level. This leads to debates about whether resources would be better allocated towards broader public health interventions.
In conclusion, the inclusion of Wegovy under Medicare points to broader debates in public health policy. While the drug could lead to direct cost savings in treating obesity-related conditions, this must be balanced against its high initial cost, potential side effects, and the broader question of addressing the overarching causes of obesity. As Medicare considers expanding coverage, it must navigate these complex waters with an eye towards both immediate benefits and long-term sustainability. Judicious use of negotiation power, careful monitoring of health outcomes, and an integrated approach to obesity that includes pharmaceuticals and public health measures will be crucial in determining the impact of this policy change.

Leave a Reply