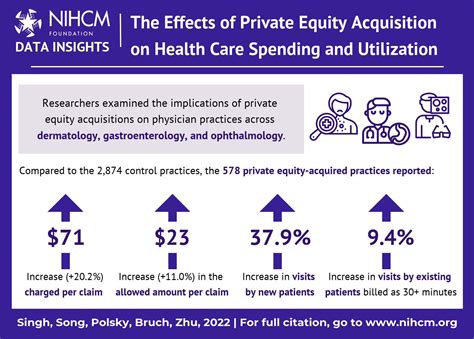
The headlines about exorbitant medical bills have become all too familiar, with patients across the United States lamenting the skyrocketing costs of healthcare. One of the major culprits behind this alarming trend is private equity (PE). Private equity firms, with their profit-maximization focus, have crept into the healthcare sector, and their influence is more insidious than it initially appears. They acquire healthcare providers, hospitals, and medical practices, implement aggressive cost-cutting measures, and significantly increase charges, all in the quest to maximize returns on their investments.
The essential issue here extends beyond private equity’s direct involvement. The healthcare system in America can be described as a ‘tragedy of the commons’ where multiple stakeholders, including insurance companies, pharmaceutical firms, and providers, all share the blame. One comment from nolongerthere aptly puts it: ‘There’s no one boogeyman to blame, it’s a very classic tragedy of the commons.’ It signifies that the root cause is multifaceted and deeply entrenched in how our healthcare system is structured. From regulatory bottlenecks to the limited choice in providers, various elements contribute to the crisis.
Llamaimperative offered a slightly different perspective, stating, “…there are many, many boogeymen, all of whom bear blame, and all of whom need to be corrected/removed/circumvented/improved.” The solution, therefore, is not straightforward and cannot be addressed by targeting just one actor. Each segment of the healthcare system—private equity, insurance companies, pharmaceutical companies, and regulatory bodies—all play significant roles. It’s a broken system that rewards inefficiencies and penalizes patients.
One substantial point discussed is the role of insurance and how it inadvertently exacerbates the problem. Commenter bluGill mentions, ‘We can’t even choose our insurance – it comes from your employer with no choice (or no real choice).’ This lack of choice results in limited competition, poor quality of care, and a system where the patient, doctor, and insurer play a constant blame game. Insurance companies might negotiate rates, but they often do so in ways that maximize their profits at the expense of patients and providers.
Meanwhile, individuals like tracker1 highlight the complexity and lack of transparency in healthcare pricing. The user points out, ‘The system sucks a lot, and for a lot of different reasons. Namely that there’s no room for individual negotiation, and there are dozens of pricing models for the same drugs, procedures, etc.’ The Byzantine nature of medical billing means consumers are often blindsided by costs. They might receive separate bills from the hospital, anesthesiologist, and radiologists weeks or months later and find it virtually impossible to decipher what they actually owe, often resulting in overpayments or disputes.
However, amid this bleak scenario, suggestions for reforms do surface. One promising model gaining traction involves direct primary care (DPC), where patients pay a monthly fee for unrestricted access to their primary care providers. Commenter infecto describes, ‘As a family of three, we pay $200 a month to have unlimited access (person, phone, text, email) to our doctor.’ This model bypasses insurance companies and aims to restore the doctor-patient relationship, reducing administrative overhead and focusing on patient care.
Looking internationally, several comments cite models in other countries that blend public and private care more effectively. Countries like the Netherlands, Switzerland, and Singapore offer systems that mandate affordable base coverage provided by private insurers, closely regulated by the government. In these systems, coverage is universal and costs are controlled, presenting a balanced approach worth considering for the U.S.
Ultimately, meaningful reform must begin with acknowledging the multiple, complex problems within the healthcare system. From regulating private equity and fostering competition among insurers to enhancing transparency in medical pricing and embracing innovative care models like DPC, the road to better healthcare is long but necessary. Policymakers must take a holistic view of the industry, combining the best practices from around the world with innovative domestic solutions. Only then can we hope to rein in costs and ensure quality care for all.

Leave a Reply